
Media
Media Coverage
-
Antimicrobial Resistance (AMR)
What are antifungal medicines? And what does antifungal resistance mean? Is it somehow related to Antimicrobial Resistance (AMR)? At first glance, these topics may seem difficult to understand. But do not worry, in this blog we will try to shed light on them.
-

Conversation with Lisa McNeil
This month we spoke to Lisa McNeil, a patient advocate for aspergillosis who is a member of the ELF Aspergillosis Patient Advisory Group (PAG). Here, she talks about this and our newest resource on antimicrobial resistance, which she helped to produce.
-

Rise of Super Fungus
An old infectious foe is returning with a vengeance: it's called ringworm. Despite the name, it is not a worm but a contagious skin fungus that can disfigure — and it has learnt how to defeat our best medicines.
-

Blackpool Woman with Rare Lung Disease Warns of Mould Risk
A woman who developed a chronic lung disease after being exposed to mould has urged people with unexplained breathing problems to "think fungus".
-

Blackpool Woman Diagnosed with a Chronic Lung Disease
Lisa McNeil, 52, was diagnosed with Aspergillus Bronchitis in 2011 – a chronic condition that causes tenacious mucus production, breathlessness, wheezing and extreme fatigue.
-

While Walking In Damp Leaves May Be Blame If You Are Out Of Breath
Why walking in damp leaves may be to blame if you’re out of breath: How mould that can be found indoors and outside.
-

NBC News
As fungal infections grow resistant to medication, desperate patients try drug after drug.
-
Resistant Aspergillosis
Resistant Aspergillosis 'Superbug' Spreading from the Environment
-

Everything is scary. Living with a rare lung condition during Covid
-

The forgotten superbug: Is it time to bring fungal infections out of the dark?
-

Aspergillosis: how environment pollution helped transform a fungal infection into a drug-resistant superbug
-

Husband who was told he might have months to live due to a condition caused by mould that grew in his lungs is still alive two years later thanks to a last-ditch drug and 'miracle' recovery
-

Ramsgate events boss defies odds after rare lung disease diagnosis
-

Patient testimony: hyper-IgE syndrome and associated lung infections
-

Talk Health - Aspergillosis – a hidden threat
-

My shocking diagnosis of aspergillosis
-

Townsville flood aftermath: Resident's relentless mould battle six months after monsoon event
-

The world's medical experts are terrified at the way antibiotics are rapidly becoming useless - but now a new swathe of vital drugs have stopped working
-

Living with allergic bronchopulmonary aspergillosis
-

Gardener who nearly lost her lung issues deadly warning
-

Compost heaps help spread killer superfungi
-

The deadly spores that could be hiding in your home or garden: Experts warn of 'serious and immediate' threat posed by drug-resistant fungi that can cause lung disease
-

European Lung Foundation - Newsletter
Aspergillosis Trust are included monthly in their newsletter
Aspergillosis Trust (AT) Registered Charity No: 1194699 – Key Messages for Media Enquiries
We keep hearing similar stories. So AT feel it is important to get these key messages across to prescribers, mainly GPs and asthma nurses in the frontline, who see patients first. Earlier diagnosis and correct treatment helps outcomes. Diagnosis is very difficult, so refer to your local respiratory centre as soon as possible.
Patients find it can take years to get a diagnosis of aspergillosis
All of us are potentially at risk until we know enough about the process of infection to say differently
Chronic forms of aspergillosis are mostly incurable, but symptoms can be effectively managed by a specialist doctor. These forms include:
allergic bronchopulmonary aspergillosis (ABPA)
chronic pulmonary aspergillosis (CPA)
severe asthma with fungal sensitivity (SAFS)
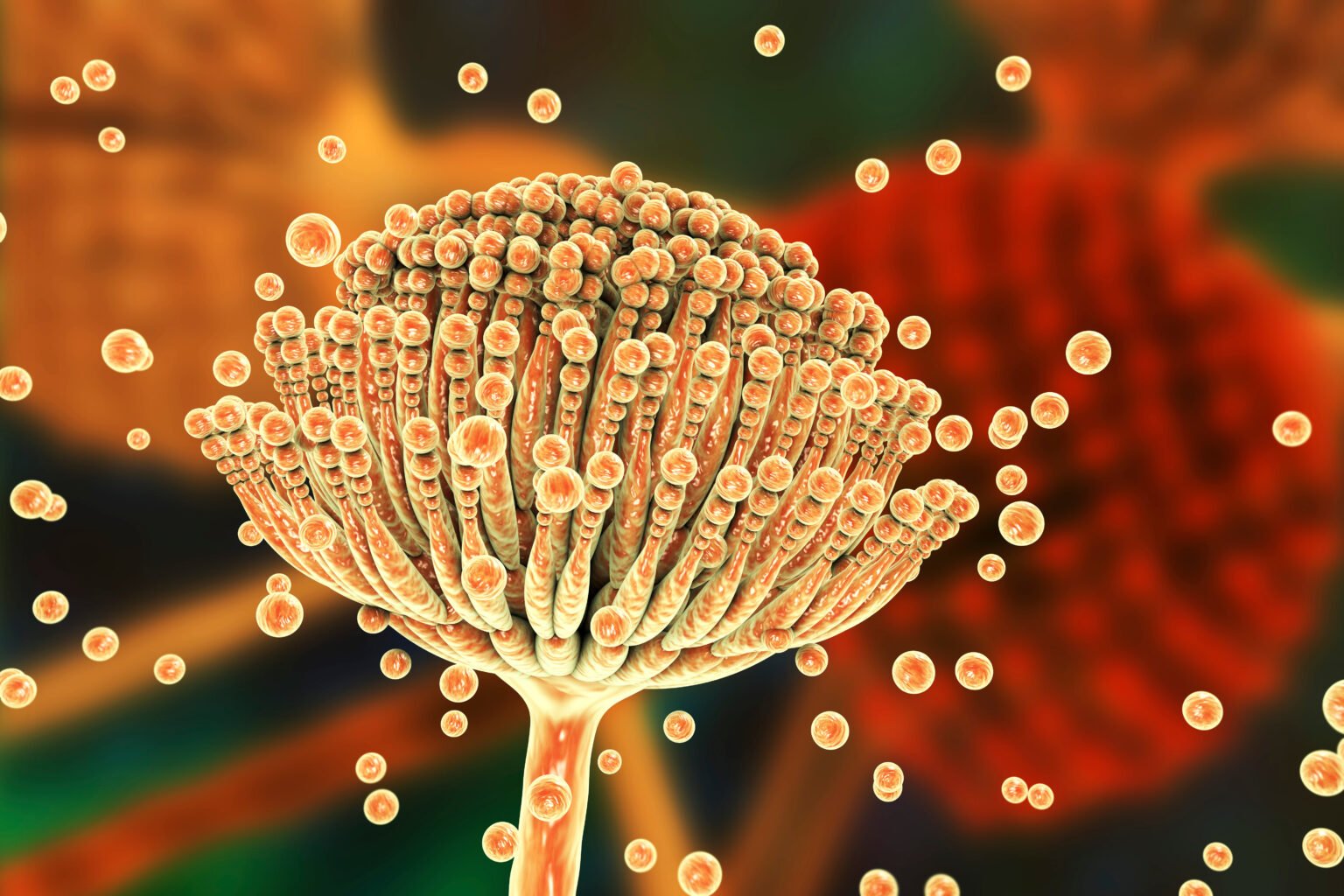
The fungus responsible for these conditions is called Aspergillus. It is estimated that aspergillosis impacts the lives of approximately this many people in the UK:
50,000 with ABPA
4000 with CPA
250,000 with SAFS
If patients are having asthma flare-ups despite using inhalers correctly, think of the possibility of fungal lung infections earlier. Aspergillosis can present as uncontrolled asthma.
If repeated attempts at treating lung infections with antibiotics fail, then think of fungal lung infections sooner. We have anecdotally heard of people having 6 months or longer of repeat courses of antibiotics, without any further investigations. Consider x-ray referrals and taking sputum samples for fungal culture, for example after two courses of antibiotics not helping resolve lung infections. Also, refer to your local respiratory specialist centre. This may help to reduce unnecessary exposure to antibiotics, therefore helping to limit antimicrobial resistance by implementing antimicrobial stewardship programmes (appropriate use of antibiotics, antifungals etc).
Chronic aspergillosis is usually a ‘hidden’ lung condition, so it often gets missed.
It can appear in a significant proportion of people with chronic obstructive pulmonary disease (COPD), tuberculosis (TB), asthma, Cystic Fibrosis (CF), sarcoidosis and occasionally in pulmonary cancer. Treatment for the accompanying disease can sometimes obscure the diagnosis of aspergillosis. The overall impact is that treatment for aspergillosis can be delayed, as the medical team concentrate on the initial diagnosis – awareness is key.
We have mostly discussed chronic aspergillosis, as these tend to be slow growing. This results in long term conditions (LTC) that affect people who are continuing their daily lives as normally as possible. Patients appear ‘healthy’ even when really ill. Aspergillosis in all its forms is seriously disabling and life changing. So refer to a specialist centre for expert guidance in managing aspergillosis.
There are also thousands of people who get acute (sudden) aspergillosis. This is a serious infection that always happens to people who are severely immunocompromised (their immune system doesn’t work properly). For example, these could be people having bone marrow (stem cell) transplants. Fungal growth is rapid and treatment must start quickly. These cases are managed in the hospital that carried out the transplant.
Aspergillosis Trust would also like to convey these points too:
Using diagnostics i.e. point of care tests (POCT) when these become available, will help to detect fungal infections earlier. Initiating correct treatment will also avoid unnecessary exposure to antibiotics. A number of point of care tests are currently available for bacterial lung infections. These are already being used in primary care by GPs and pharmacists.
Being aware that antifungals can interact with many other prescription medicines, which can affect levels of either medicine. This can lead to toxicity or alternatively low levels of antifungal and even fungal resistance. Whether you are a doctor or patient, please check for interactions at http://www.antifungalinteractions.org
Highly Specialist Centres in the UK
The National Aspergillosis Centre, (NAC) is funded by the UK Highly Specialised Clinical Commissioning Group. This is to provide services to the NHS for chronic pulmonary aspergillosis (CPA). NAC is currently delivered by Wythenshawe Hospital, MFT, Manchester. This service is led by Dr Caroline Baxter, Respiratory Consultant, Acting Clinical Director of NAC. It is fully funded for use by NHS patients with CPA. Most antifungal medication is available at no cost to your local service, or clinical commissioning group (CCG). NAC also treats other forms of chronic aspergillosis eg. ABPA, SAFS as a regular NHS service. So your local CCG will incur costs for these. A referral from an NHS doctor is required to access all services. http://www.nationalaspergillosiscentre.org
There are other respiratory specialist centres throughout the UK and worldwide (see link below) They also have the expertise in diagnosing and treating chronic aspergillosis, but are not linked to the NAC. These included the Royal Brompton and Harefield NHS Trust. The aspergillosis clinic is run by Dr Darius Armstrong-James, honorary consultant physician in Infectious Diseases and Medical Mycology. He is also a Clinical Senior Lecturer at the National Heart and Lung Institute, Imperial College, London.
https://aspergillosis.org/aspergillosis-specialist-centres/
For more details contact our press officers on jill@aspergillosistrust.org or cliff@aspergillosistrust.org


